Jaundice:
the Yellow Peril
by Kenneth Lyen

Yellow Peril
When I was in England in the 1960s, British children would point at me and yell “Yellow Peril!” That is what they called the Chinese and Japanese. Over the decades, this form of prejudice has gradually faded. So I am now borrowing the phrase to point my finger at another form of "yellow peril", namely severe jaundice in the newborn.

What is Newborn Jaundice?
Jaundice is the yellowish-orange discoloration of the skin and sometimes the eye-white.
What is Physiological Jaundice?
The term “physiological” refers the normal jaundice that most babies experience. It commonly develops after the second or third day after birth, reaches a maximum around the fifth day and subsides soon after that. The urine may be a light yellow, and the stools are mustard yellow or darker in color. Up to 60% of normal babies become visibly jaundiced.
Apart from the yellow discoloration there are usually no other symptoms. This type of jaundice does not cause any medical problems.
The level of bilirubin does not cross into the abnormal range which is 200 umol/l on day 2 of life, and above 250 umol/l after day 3 (see table below).

Factors Predisposing to Newborn Physiological Jaundice
Before birth, while inside the womb, the foetus gets oxygen from mother which diffuses from the uterus to the placenta. Because mother has used up some of the oxygen for herself, and the diffusion process is not very efficient, baby may not be receiving very much oxygen. In order to secure as much oxygen as possible, baby increases its red cell production so that the increased haemoglobin can bind to as much oxygen as possible.
At birth, baby cries, breathes air, and has access to an almost unlimited supply of atmospheric oxygen. There is therefore no need for it to have so much haemoglobin, it breaks down the surplus red blood cells. This destruction takes place in the spleen.

The haemoglobin is separated into haem, globin, and iron. The latter is recycled, and the haem is converted into bilirubin, the chemical pigment of jaundice. The rapidity of breakdown of haemoglobin and its conversion into bilirubin will be one of the factors determining the degree of jaundice.
Unconjugated and Conjugated Bilirubin
The bilirubin produced in the spleen and enters the bloodstream, and it is unconjugated, meaning that it is not bound either to albumin, or to a sugar known as uridine diphosphate (UDP) glucuronic acid. The latter binding takes place in the liver where two molecules of UDP glucuronic acid binds to bilirubin, producing bilirubin diglucuronide. The bilirubin is now conjugated.
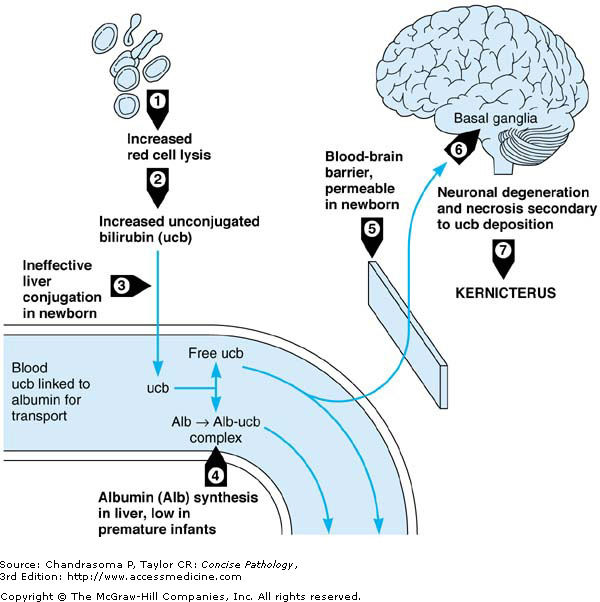
The difference between unconjugated and conjugated bilirubin is important. The unconjugated bilirubin is water insoluble and fat soluble, meaning that it can penetrate the barrier protecting the brain, known as the blood-brain barrier. In contrast, the conjugated bilirubin is water soluble but fat insoluble, and this bilirubin cannot readily penetrate the blood-brain barrier.

There is a potential problem in the first week of life. The liver does not handle the conjugation process very efficiently, and is said to be immature. Coupled with the larger quantity of unconjugated bilirubin coming from the spleen, there is double jeopardy.

Measurement of Jaundice Level
There are two common ways of determining the degree of jaundice. The first is to extract some blood from a heelprick puncture and collecting it into a capillary tube. The laboratory centrifuges the blood and measures the serum bilirubin. An alternative non-invasive method is to use a handheld transcutaneous bilirubinometer which measures the yellowness of the skin.
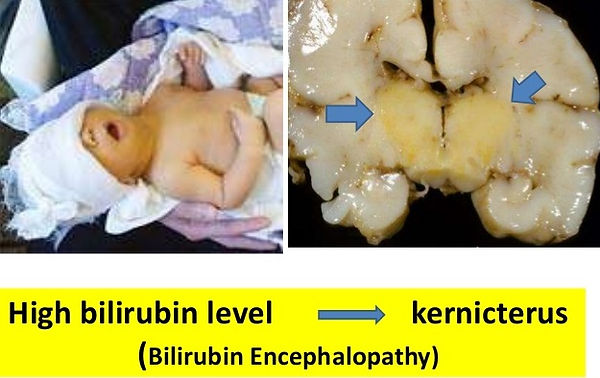
Kernicterus
This is a severe and dangerous form of jaundice. Babies are very deeply yellow, and the white of the eyes becomes an orange-yellow color. There may be feeding problems, fussiness, restlessness, lethargy, difficulty waking from sleep, and a high-pitched cry. The baby may be floppy, with episodes of increased muscle tone. Some may arch their head and neck backwards, known medically as opisthotonos.
The cardinal sign, the involuntary movements, may not show up until a few years of age. Kernicterus is characterized by uncontrollable movements known as athetosis. The arms, legs, and neck have a slow twisting squirming movement, which subsides during sleep. However, there may be painful muscle spasms at night.
Some individuals have speech delay which can either be due to hearing loss or intellectual disability. The eyes may have a tendency to deviate upwards. The enamel of the teeth may be poorly formed.

Pathology of Kernicterus
Unconjugated bilirubin is deposited throughout the brain, but in kernicterus, it has a predilection for the basal ganglia an area that coordinates muscle movements, the eighth cranial nerve which is responsible for hearing, and the frontal cortex where intelligence resides.

Noraini bte Adnan
I have known Noraini bte Adnan for over 30 years. Her parents brought her to see me in my clinic when she was a young child. She suffered from kernicterus, a disease caused by severe neonatal jaundice. Although she received an exchange transfusion on her third day of life, it was too late, and severe jaundice damaged her brain.
She had the involuntary writhing movements of the limbs and trunk, and did not develop the two other problems that often accompany kernicterus, namely hearing loss and intellectual disability. She hears very well, and her intellect is first rate, enabling her to write for journals published by organizations supporting people with disabilities.
Noraini’s athetosis is quite a handicap because she cannot walk and can only move around using a motorized wheelchair. She has difficulty keeping her hands steady and this prevents her from holding a cup without spilling the drink; fork and spoon will miss her mouth, so food does not get eaten. Dressing herself, toileting, bathing, and transferring from wheelchair to bed at night is impossible without help.
On the positive side, she has a heart of gold, and she goes out of her way to help other physically challenged persons by volunteering with organizations, like the Disabled Peoples Association of Singapore.

Breast-fed Jaundice
Breast-fed babies may have more prominent jaundice, which can persist for3 months or longer. There are several explanations for breast-milk jaundice, all of which result in preventing the normal conjugation of bilirubin.
-
It may be due to an enzyme in breast milk called glucuronidase which deconjugates the conjugated bilirubin.
-
It may also be due to the presence in breast milk a metabolite of progesterone called 3-alpha-20-beta pregnanediol which inhibits the action of the enzyme uridine diphosphoglucuronic acid glucuronyl transferase which is responsible for conjugation.
-
A third explanation is the presence of lipoprotein lipase in breastfed babies, which increases the production of nonesterified free fatty acids that also inhibits hepatic glucuronyl transferase, resulting in reduced conjugation and subsequent decreased excretion of bilirubin.
Current recommendations for jaundiced breast-fed babies is to monitor the bilirubin level, and if it is below 200 umol/l, mothers should continue breast feeding. They are also advised to feed more frequently, or to add extra water in between breast feeds.

Glucose-6-Phosphate Dehydrogenase (G6PD) Deficiency
About 3% of babies boys born in Singapore have an inherited absence of the enzyme glucose-6-phosphate dehydrogenase (G6PD) in their red blood cells. This predisposes them to severe jaundice which can be manifest even in the first day of life. G6PD is an enzyme in the body that helps keep the red blood cells in a reduced state.

Inheritance of G6PD Deficiency
The mode of inheritance of G6PD deficiency Is sex-linked recessive, meaning that boys are affected mainly, and girls rarely have the condition. However, females carry the gene, and they can pass it to their male children.
G6PD deficiency is a major cause of severe jaundice in Singapore, and in the 1960s was the number one cause of death in babies under one week of age, and also the major cause of cerebral palsy and intellectual disability. It led paediatrician Professor Wong Hock Boon and his team to develop nationwide screening of cord blood for G6PD deficiency, and this has led to measures to monitor babies very closely, resulting in a dramatic fall in the number of cases of kernicterus.

Quinine and G6PD Deficiency
There are several triggers of jaundice in G6PD deficient individuals.

One of the earlier drugs that caused severe jaundice and haemolytic anaemia was quinine. This antimalarial is obtained from the bark of the cinchona tree. In the 17th century, Jesuit missionaries in Peru brought it back to the West.

During the second world war, American soldiers fighting the Japanese in the Pacific war arena were given chloroquine as a preventive measure to protect them from malaria. The African-Americans who had G6PD deficiency developed haemolytic jaundice.

Fava Beans
Fava beans are known to trigger haemolysis in G6PD deficient individuals. Indeed G6PD in the Mediterranean was referred to as favism.

Pythagoras
The most famous ancient Greek mathematician with G6PD deficiency is Pythagoras. He would not allow his followers to consume fava beans, saying that it would “sicken them”.

Evolutionary Advantage of G6PD Deficiency
Borrowing the idea from sickle cell anaemia, it has been postulated that the high frequency of G6PD deficiency in hot climates especially where malaria is prevalent, may perhaps be due to G6PD deficiency conferring an advantage to survive malaria.

ABO and Rhesus Incompatibility
If a mother with a Rhesus negative blood type carries a baby with Rhesus positive blood group, some of the baby’s blood crosses into mother during delivery. Mother will develop anti-Rhesus antibodies, but the first child escapes from the effects of these antibodies because the child is born before mother makes enough antibodies. However, if mother has a second child with Rhesus positive blood, when this baby’s blood crosses the placenta into mother, she will produce antibodies more rapidly, and these will cross back into the fetus, damaging the baby’s red blood cells.

We could have prevented the second child developing haemolytic jaundice if, after the birth of the first child, we injected anti-Rhesus antibodies (Rhogam) into mother. The antibody binds to the few Rhesus positive cells from the baby that have crossed into mother, and thereby prevents mother recognizing these cells. She therefore does not develop a primary immune response to Rhesus, and so the second child will not stimulate a secondary immune response. After delivery of the second child, mother needs to have another injection of Rhogam to protect her third child.

Familial Jaundice
One of my medical students pointed out to me that the entire Simpson’s family seemed to be a bit jaundiced. That made me think of other familial causes of jaundice, although not everyone in the family necessarily develop the jaundice. The two that immediately came to mind are:

1. Gilbert Syndrome
Gilbert's syndrome is a mild disorder, inherited as an autosomal recessive. It is due to a genetic mutation causing slightly decreased activity of the bilirubin uridine diphosphate glucuronosyltransferase (UGT1A1) enzyme. This leads to raised the failure of the liver to conjugate bilirubin and hence a rise in blood levels of unconjugated bilirubin. There is generally no need for treatment of the relatively mild jaundice.
2. Crigler-Najjar Syndrome
Crigler-Najjar Syndrome is a much more severe disorder, inherited as an autosomal recessive and sometimes as an autosomal dominant. It is due to a defect in the gene coding for uridine diphosphate glucuronosyltransferase (UGT1A1) enzyme. There is failure of conjugation of bilirubin resulting in dangerously high levels of unconjugated bilirubin resulting in kernicterus. Treatment requires prolonged phototherapy, exchange transfusion, but eventually liver transplantation may be the ultimate solution.

Phototherapy
The current best treatment of treating newborn jaundice is phototherapy. It was discovered by accident at Rochford General Hospital, Essex, England in 1956. Blood taken from jaundiced babies and placed in test tubes had less bilirubin, and nurses noted that babies placed under the sun were less jaundiced. In 1968, a paper publishing the results of a randomized clinical trial confirmed the efficacy of solar therapy. However it took another decade before the practice was accepted more widely. It was found that the optimal wavelength of the light was in the visible blue spectrum between 460-490 nm range.

The mechanism of action of phototherapy is the conversion of bilirubin into its structural isomer known as Z-lumirubin. This isomer is relatively fat insoluble and water soluble, so that it does not cross into the brain, and is more readily excreted in the urine.

We can now deliver phototherapy using a biliblanket. This is popular with families because the biliblanket can be rented and used at home.

Exchange Transfusion
Before phototherapy was widely used, the standard treatment for severe jaundice was exchange transfusion. Blood was extracted from the baby and replaced with compatible adult blood. This practice has declined over the decades, but may still be necessary if there is a power cut so that phototherapy is not available, or if the bilirubin is dangerously high, in excess of 300 umol/l.


Conclusions
Kernicterus is a preventable disorder, and it needs one to be very vigilant with neonatal jaundice. With the availability of handheld transcutaneous bilirubinometer, all newborn babies can be screened daily for jaundice. Phototherapy can be effectively delivered at home using the biliblanket. Kernicterus should become extinct with these simple procedures. No more yellow peril!
The above video is a very good overview of polio. It can also be viewed online:
https://www.youtube.com/watch?v=dJ_dasmimE4
Creative Commons CC BY-SA 4.0
The above video is an excellent overview of polio. It can also be viewed online:
https://www.youtube.com/watch?v=6akhmBqAe2g
Creative Commons CC BY-SA 4.0
References
Movement disorders due to bilirubin toxicity https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4388741/
Phototherapy for jaundice: https://emedicine.medscape.com/article/1894477-overview
Videos
Bilirubin Metabolism: https://www.youtube.com/watch?v=dJ_dasmimE4
Jaundice: https://www.youtube.com/watch?v=gIACp5js4MU
Neonatal Hyperbilirubinaemia: https://www.youtube.com/watch?v=jIYUmne4fc0
Kernicterus: https://www.youtube.com/watch?v=EOWdgXuUQbQ
Kernicterus: https://www.youtube.com/watch?v=nelPuohNTUk
Written by Kenneth Lyen
31 October 2018, updated 27 April 2019